The Evolution of Depression
How depression might—or might not—be a biological adaptation
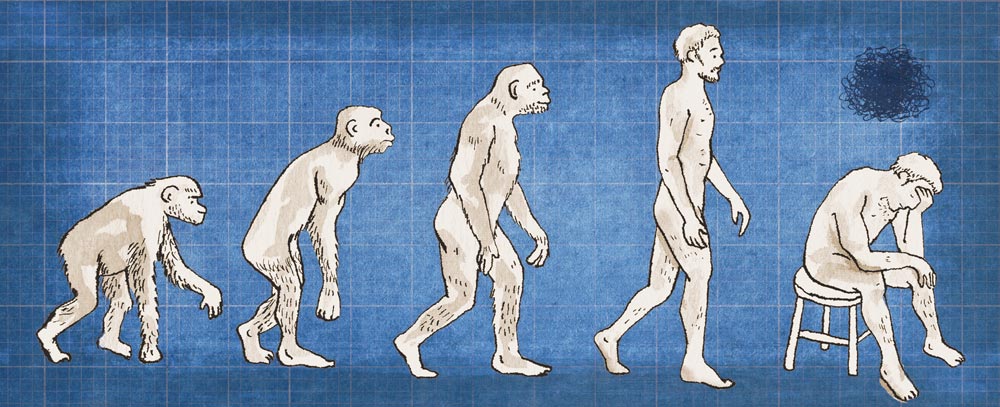
Since the dawn of the species about 200,000 years ago, humans have evolved in response to the environments in which they’ve found themselves. In Northern Europe, lighter skin helped early inhabitants get enough vitamin D during the dark winters. In places in Africa plagued by malaria, many people have a genetic mutation that makes them immune. Like all living things since the first protozoa, the human body has been shaped by natural selection. And evolutionary psychology suggests that the mind has as well. Evolutionary psychologists look for the advantages of different behaviors and mental traits that might cause them to spread through the population.
For more than 30 years, UVA psychiatrist Dr. Andy Thomson (Med ’74) has been treating patients, and most often he treats them for depression. Major depressive disorder is one of the most common mental disorders in the United States, and each year clinical depression affects more than 17 million Americans.
Thomson and his collaborator Paul Andrews, now at McMaster University in Canada, believe that depression is an evolutionary paradox. If it didn’t confer any advantages, it should have been selected against and occur only rarely in the population. What kind of evolutionary advantage might depression have?
“Depression, psychic pain, alerts you to the fact that you have a problem, stops business as usual, focuses your attention,and can provide a signaling function that you need help,” says Thomson. “Basically, it forces you to think. Now with all its stressors and the myriad ways of evading them, modern life doesn’t encourage you to think deeply. But thinking deeply works. It’s doing what the mind was made to do.”
He and Andrews went looking for evidence that rumination—focused meditation on a problem, common in depressed people—might confer some advantages on depressed people. First, the pair focused on neuroscience. Our ability to concentrate, they wrote in a 2009 article published in Psychological Review, largely reflects activity in the brain’s left ventrolateral prefrontal cortex. Neurons there must continuously fire to keep our attention on track. In depressed patients, such activity increases. That “revving up” amplifies working memory, which facilitates slow, difficult, analytical thinking that can be used to solve problems.
A few other studies support the hypothesis that depressed people outperform nondepressed people at certain mental tasks. In an Australian experiment, shoppers exiting a checkout line were tested to see how accurately they remembered items they’d just seen. Those who reported their moods as low recalled nearly four times as many of the items.
In a German study published in the Journal of Abnormal Psychology, groups of healthy or hospitalized depressed people played a decision-making computer game with the goal of hiring the best applicant in a simulated job search. Nondepressed subjects stopped going through the list of applicants earlier than depressed subjects, so the depressed subjects were more likely to hire the best applicant.
The suggestion that depression might have a purpose is unorthodox. Thomson’s and Andrews’ novel ideas have garnered attention from the Scientific American Mind and the New York Times Magazine. “Absolutely, it’s controversial,” Thomson says. “It completely challenges current orthodoxy in its model of depression and the current standard of care for it.”
“The primary question we should ask is: ‘How is one defining depression?’” says Dr. J. Kim Penberthy, a clinical psychologist and associate professor in the department of psychiatry and neurobehavioral sciences at UVA. “Depression can be defined in multiple ways and there is a spectrum of severity of depression.” Symptoms range from a low mood to chronic, severe and incapacitating clinical depression. She says that some depressive feelings are appropriate and temporary normal responses to losses or bad situations. “However, severe or chronic depressions, by definition, interfere significantly with a person’s ability to function in day-to-day life.”
Ruminative thinking that accompanies clinical depression, she says, has been shown to impair thinking and problem solving. “In fact, mindfulness-based psychotherapies directly challenge rumination in depression and have been found to be very successful in preventing relapse in clinical depression,” says Penberthy
In contrast, Thomson argues that recovery may actually require ruminative thinking to solve the problems that trigger depression. “When you have the pain of a fish hook in your hand or a high fever from the flu, it interferes with work and your ability to function day-to-day,” Thomson says. “The pain and the fever are functional; they help solve the problems.”
A study at an interuniversity research institute in Japan found that people diagnosed with major depression showed decreased metabolic activity in their frontal brain regions—the problem-solving parts of the brain—compared with healthy control subjects.
Thomson notes that decreased metabolic activity in these studies is usually aerobic. “But there is evidence that with the shift to sustained concentration in depression there is a shift to anaerobic, lactate-based metabolism to sustain the neuronal effort,” says Thomson.
Penberthy cites a review article by Dr. Charles DeBattista that concludes that “the types of executive deficits seen in depression include problems with planning, initiating and completing goal-directed activities” and that such “executive dysfunction” tends to worsen in direct proportion to the severity of depression.
Penberthy also says that depression isn’t entirely caused by genes, and thus calls into question whether evolutionary psychology is a helpful tool for understanding it. “Clinical depression is conceptualized by clinicians and researchers as having a biopsychosocial etiology, meaning that it is caused by a combination of biological, psychological and social—or environmental or cultural—factors.” She explains that people likely have some genetic predisposition to unipolar and bipolar depression, and these kinds of depression may run in families. But clinical depression has also been associated with early physical or psychological trauma, such as abuse or neglect, as well as repeated psychological insults later in life.
Thomson says that evolutionary psychology is inclusive of biopsychosocial causes. He suggests an analogy, “If you have an infection, you have the latent ability to respond with fever,” he says. Trauma can be compared to an infection and depression may be our latent ability to respond to it, like a fever.
During the last 200,000 years, the human brain has grown larger as men and women have navigated an increasingly complex human society and an often-dangerous natural environment. It seems reasonable that responding to difficult circumstances—a drought, a family conflict—with genuine sadness and deep, concentrated thought would be adaptive.
“But clinical depression is a very different thing,” says Penberthy, “and research suggests that it is hardly an adaptive state of being.”
“Like pain, depression can malfunction,” says Thomson. “We never say all depression is adaptive.” Thomson points out that although grief and depression have very similar symptoms, depression is considered a disease, while grief is not. “It’s just another indication,” he says, “of my profession’s confusion about the fundamental design and function of depression.”